What Is an Obesity Medicine Physician?
A board-certified obesity medicine specialist is a physician who has proven competency and understanding of the complex genetic, environmental, social, biologic, and behavioral factors involved in the lifelong disease named obesity. They specialize in helping patients lose weight, maintain that weight loss, and control or treat the various medical conditions associated with excess weight.
The two main organization for obesity medicine are the Obesity Medical Association for physicians, and the national research organization The Obesity Society, which includes physicians, psychologists, registered dietitians, public health specialists and research scientists in many areas such as genetics, nutrition and behavior.
An obesity medicine physician is extensively trained to use a comprehensive approach which includes diet, physical activity, behavioral changes and pharmacotherapy. They help with the pre- and post-surgical care of bariatric surgery patients. We have found that obesity medicine physicians are invaluable to give long-term help to these bariatric surgery patients to minimize or prevent any weight regain before it happens and to minimize or prevent any late post-surgical vitamin or nutrient deficiencies.
Obesity medicine specialists also focus on health policies about the prevention of obesity and minimizing weight bias. They work with psychologists, psychiatrists, registered dietitians and exercise physiologist to help in the treatment of this complex disease.
To become board certified in the subspecialty of obesity medicine, a physician first be board certified in a medicine specialty (for example pediatrics, family medicine, psychiatry) and then pass a nationally created and scored exam. This exam is given by the American Board of Obesity Medicine and the questions are from nationally recognized experts in the field of obesity. To be able to take this exam, physicians must prove that they’ve taken at least 65 hours of specialized continuing medical education in obesity medicine. They must recertify every 10 years.
Why Choose an Obesity Medicine Specialist?
Any licensed physician, nurse practitioner, physician’s assistant or chiropractor can advertise and offer a “medical” weight loss program. Only physicians who have done the training to become board-certified in obesity medicine have proven that they have a background of extensive hours of training in the scientific study of the disease of obesity. They have the knowledge, tools and techniques to design a specialized medical weight loss programs tailored to the needs of individual patients and then modify them as the treatment progresses. These personally-designed programs provide the wisest and safest way to lose weight and maintain that loss.
What Is Obesity and Why Do You Call It a Disease?
Obesity is scientifically defined by 3 criteria (With BMI used most commonly):
- BMI (weight in pounds divided by height in inches) ratio of 30 or greater.
- Percent Body Fat of greater than 25% in men or greater than 32% in women.
- Abdominal Obesity is a waist circumference of greater than 40 inches in men or greater than 35 inches in women.
Obesity Algorithm®. ©2017-2018 Obesity Medicine Association
The word “obese” is an old word from OB (over) and Ese (to eat).
Obesity is a chronic disease that has multiple causes. It is chronic, and it is a neurobehavioral dysfunction where increased body fat promotes dysfunction of body fat cells leading to metabolic, biomechanical and psychosocial health consequences.
Or more simply, as our bodies carry more and more energy storage cells (fat cells) we become resistant to fullness signaling, we have increased biochemical changes that lead to joint destruction, breathing problems, diabetes, heart attacks and strokes. More than that, this disease is frequently a lifelong relapsing problem of weight gain exacerbations set off by physical, emotional, hormonal, neurologic and other signals. It has some proven genetic and epigenetic causes.
“Obesity is defined as a chronic, relapsing, multi-factorial, neurobehavioral disease, wherein an increase in body fat promotes adipose tissue dysfunction and abnormal fat mass physical forces, resulting in adverse metabolic, biomechanical, and psychosocial health consequences.”
Obesity Algorithm®. ©2017-2018 Obesity Medicine Association
How Much Should I Expect to Lose?
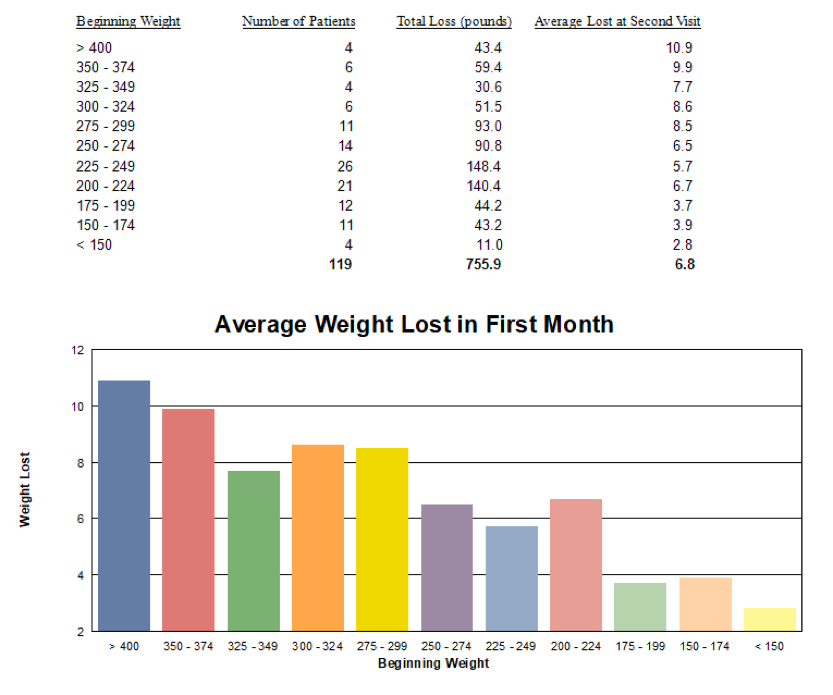
The average weight loss after 2 weeks on the program is 6.8 lbs.
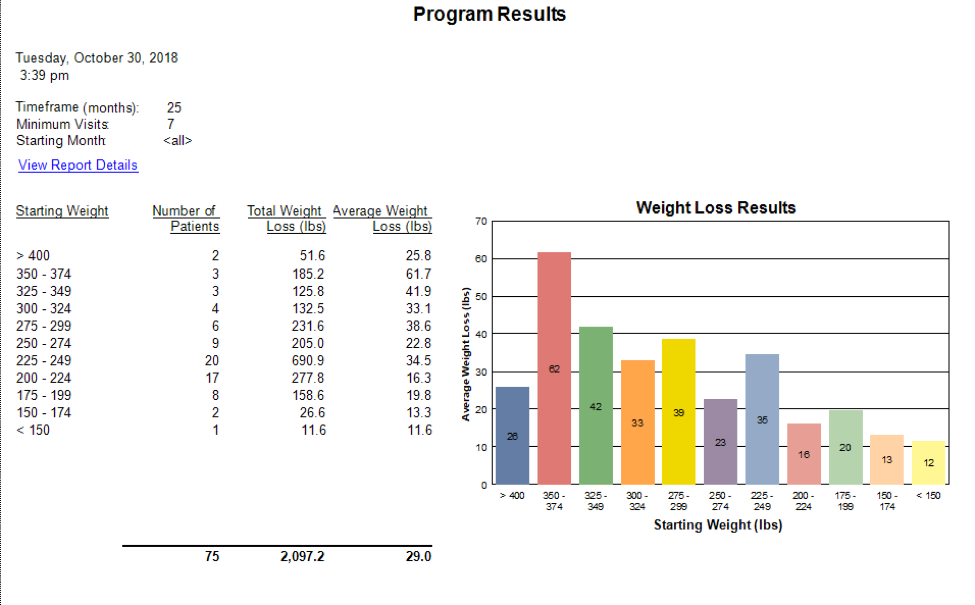
The average weight loss for people who remained on the program for at least 7 visits (about 18-20 weeks) was 29 lbs. People with a starting weight 250 and above — average weight loss was 34.5 lbs. 300 and above — average was 41.3 lbs.
What Medicines Do You Use?
In obesity medicine, our specialty and the available medicines is evolving very rapidly. We are called the science of hope for overweight and obese people. We treat various aspects of the patient’s needs with different medicines.
The first need is to reduce the person’s hunger, which we do with a specialized eating program (diet), supplements and prescription medicine. We also focus on correcting the inability to get full—most people with the disease of obesity are hungry all the time.
The oldest and most commonly used medication is Adipex or phentermine, and we adjust the timing or amount of this medicine depending on the patient’s history, physical size and age. Two other prescription medicines in the same class that we use them if the phentermine does not fit the patient’s needs are Bontril —phendimetrazine or Tenuate—diethylpropion.
Other prescription medicines or supplements are used to further decrease appetite, increase fullness or decrease blood insulin levels. We help decrease salt or sweet cravings, decrease binge eating patterns or night eating patterns with medications originally used for seizures or depression.
The exciting new medicines available include Qsymia, Contrave, Saxenda and Wegovy. These are approved to use for years. They are more expensive, but can be the perfect choice of the right patient. There are several new medicines in research that will be available in the next few years to give us more choices.
Our obesity-focused specialized training gives a better understanding of how to adjust and/or combine various medicines to achieve the best results for the individual patient.
The disease of obesity as a complex long-term medical condition like diabetes, hypertension, and many others. Just as your primary care physician adjusts your diabetes, or blood pressure medicines when needed as the disease changes, you need your obesity medicine specialist to make the same adjustments as your body, your environment and your disease process changes.
What Ages Do You Treat?
Currently, we see patients age 10 to 65. Younger or Older patients need to be screened on an individual basis to see if they may have benefit from medical weight reduction.
What If I Have Already Had Surgery?
Prior bariatric surgery does not change how we treat and the results we have but it does affect the nutritional needs of the patients and we discuss this during the first 1-2 visits. Currently, it is being recommended that after bariatric surgery when hunger returns and the patient starts any weight regain that they see a specialist in obesity medicine to prevent or minimize the later rebound weight gain.
I have several post-surgical patients who come in after a large or a small weight regain to prevent further gain and lose any weight regained. At GMOS clinic, we have several people who have lost weight regained after bariatric surgery.
Please realize with any medical conditions there are multiple outcomes, and no one can guarantee any amount of weight loss or any guarantee of a permanent solution to any medical problem (just like no one is going to guarantee you never have a heart attack or that your diabetes will resolve and never come back).
What If I Have Lost Weight Either Through Medical Therapy or Surgery but I Am Starting to Gain It Back?
99.9% of my patients are people who have fought the weight loss/weight regain battle for several years. Some of my patients have previously lost and regained hundreds of pounds. Now that we treat obesity no different as any chronic disease such as diabetes, hypertension, or congestive heart failure, we know that long-term pharmacologic therapy (medicines) and continuing adjustment of these medicines as the body changes is vital to the best care of people with this disease. Also, there is exceptional value in learning how our psychological and social lives also worsen our weight. And, continuing to become better and better at making food and lifestyle changes that put our patients in the healthiest physical condition we can.
Please realize with any medical conditions there are multiple outcomes, and no one can guarantee any amount of weight loss or any guarantee of a permanent solution to any medical problem (just like no one is going to guarantee you never have a heart attack or that your diabetes will resolve and never come back).